What are SOAP Notes?
SOAP notes are a standardized format used by healthcare professionals to document patient encounters. The acronym stands for Subjective, Objective, Assessment, and Plan, representing the key components of each note.
These notes provide a structured framework for recording patient information, ensuring that important details are captured clearly and concisely.
Why are SOAP Notes Important?
SOAP notes are vital in healthcare for several reasons, including:
Clear Communication
One of the primary benefits of SOAP notes is their role in facilitating clear communication among healthcare providers. By following a standardized format, SOAP notes ensure that all team members have access to the same information about a patient’s condition, treatment plan, and progress.
Legal and Professional Requirements
Proper documentation is essential in meeting legal and professional standards in healthcare. SOAP notes provide a structured format that helps ensure that all relevant information is documented, protecting both the patient and the healthcare provider in case of legal disputes or audits.
Enhanced Patient Care
SOAP notes contribute to improved patient care by creating a comprehensive record of each patient encounter. This record allows healthcare providers to track changes in the patient’s condition over time, identify trends, and make informed decisions about their care.
Quality Improvement
By organizing information into specific sections, SOAP notes promote thorough documentation and critical thinking. This approach can help identify areas for improvement in clinical practice, leading to enhanced patient outcomes and overall quality improvement in healthcare delivery.
Support for Clinical Reasoning
The structured format of SOAP notes supports clinical reasoning by guiding healthcare providers through a systematic approach to gathering, analyzing, and interpreting patient information. This method helps providers make more informed decisions about diagnosis and treatment.
Enhanced Continuity of Care
SOAP notes play a crucial role in ensuring continuity of care for patients. By providing a standardized format for documenting patient encounters, these notes help maintain consistency in treatment plans, even when multiple providers are involved in a patient’s care.
Research and Data Analysis
SOAP notes provide valuable data for research purposes, quality improvement initiatives, and data analysis. The structured format of these notes makes it easier to extract and analyze information, supporting evidence-based practice and contributing to better healthcare outcomes.
Patient Education
SOAP notes can also serve as a valuable tool for patient education. By providing a clear and organized record of the patient’s condition, treatment plan, and progress, these notes help patients understand their health status and actively participate in their care.
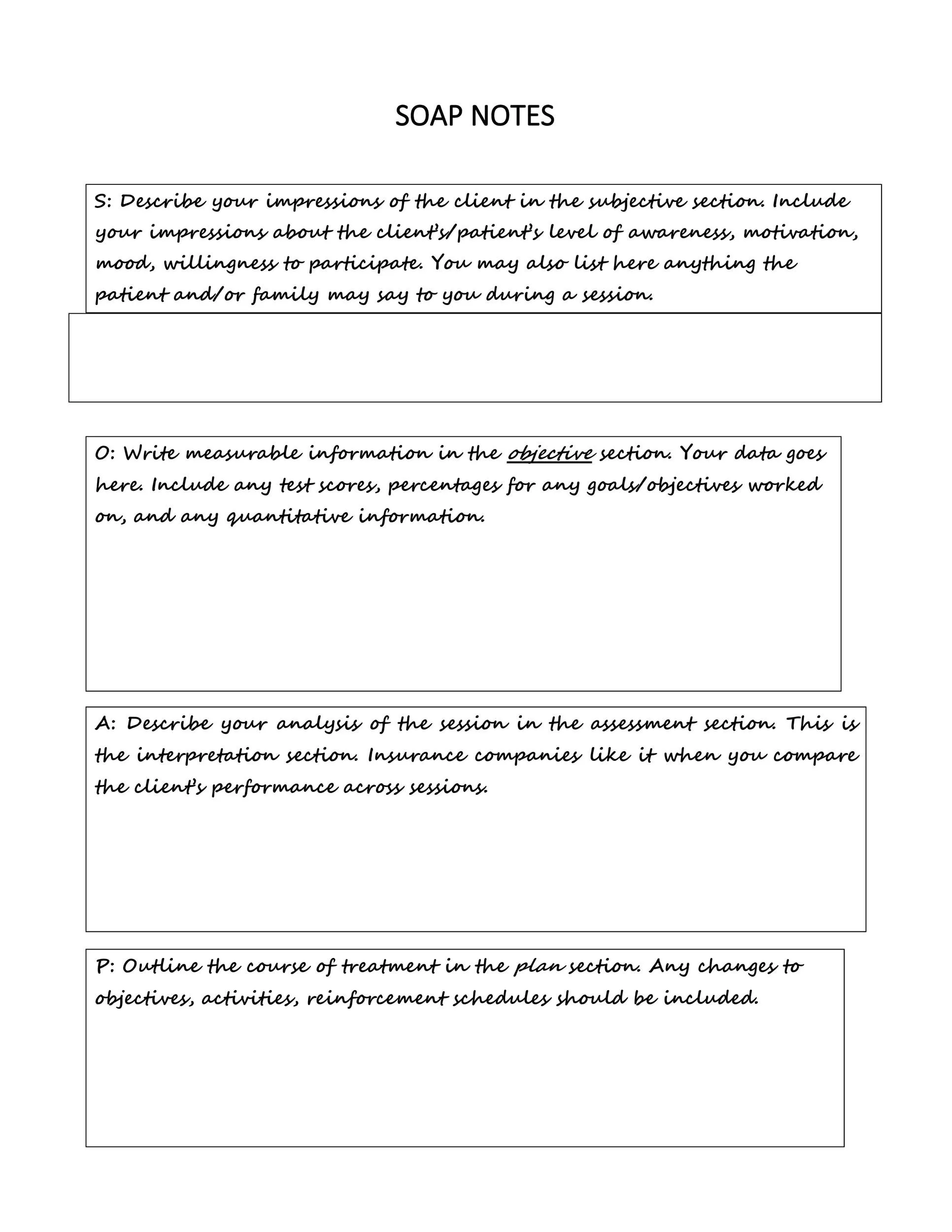
Key Elements of SOAP Notes
Each section of a SOAP note serves a specific purpose and includes essential elements:
The Subjective Section
In the subjective section, healthcare providers document information provided by the patient, including their chief complaints, symptoms, medical history, and any other relevant details. This section is crucial for understanding the patient’s perspective and tailoring the care plan to their needs.
The Objective Section
The objective section of a SOAP note includes measurable data obtained during the physical examination, laboratory tests, imaging studies, and other objective assessments. This section provides concrete evidence to support the provider’s clinical impressions and treatment decisions.
The Assessment Section
In the assessment section, healthcare providers interpret the subjective and objective information to formulate a diagnosis or assessment of the patient’s condition. This section should include differential diagnoses, the provider’s clinical impression, and any hypotheses about the underlying cause of the patient’s symptoms.
The Plan Section
The plan section outlines the treatment plan and next steps for the patient’s care. This includes medications prescribed, procedures scheduled, referrals made, follow-up appointments arranged, and any patient education provided. The plan section serves as a roadmap for ongoing care and helps ensure that all aspects of the treatment plan are addressed.
How to Write Effective SOAP Notes
Follow these tips for successful documentation:
Be Clear and Concise
When writing SOAP notes, use clear and concise language to convey information accurately and effectively. Avoid using unnecessary jargon or complex terminology that may confuse readers or other healthcare providers.
Include Relevant Information
Focus on including relevant information that is essential for understanding the patient’s condition, making a diagnosis, and developing a treatment plan. Prioritize information that directly contributes to the patient’s care and outcomes.
Use Standard Terminology
Stick to commonly accepted medical terminology and abbreviations when documenting information in SOAP notes. Consistency in terminology helps ensure that all members of the healthcare team can easily understand and interpret the notes.
Document in Real Time
Write SOAP notes as soon as possible after the patient encounter to ensure accuracy and completeness. Documenting in real time helps capture details while they are fresh in your mind and reduces the risk of forgetting important information.
Review and Update Regularly
Periodically review and update your SOAP notes to reflect changes in the patient’s condition, treatment plan, or response to interventions. Regularly updating notes ensures that the information remains current and relevant for ongoing care.
SOAP Note Template – WORD